Summary
Severe COVID often presents with repeated bouts of cytokine storm and clotting waves. Both will ultimately result in increased pulse rates (PR) and decreased oxygen saturation (SpO2). But the trigger points are different. And the clinical consequences of ignoring one vs the other will likely manifest in different post acute COVID sequelae. Cytokine waves occur without regard to time of day. Clotting generally occurs during the overnight hours when clotting factors are elevated.
Aspirin (ASA) alone likely will be insufficient to prevent pulmonary microvascular thrombogenesis. If you don't have access to clopidogrel, enoxaparin or rivaroxaban, you will need to physically anticoagulate yourself through aggressive walking to prevent lung injury and decreased O2 sats if you begin experiencing active clotting.
Here's how to read oximetry measured at rest to differentiate between the two waves:
CYTOKINE WAVES: SpO2 declines markedly (e.g., into 80s) from baseline (e.g., 95%) while PR remains stable (e.g., 84 BPM). Inaction generally results in persistent hypoxemia as PR naturally rises within 30-60 seconds to try to restore baseline SpO2, but will often fail to do so. Symptoms consistent with systemic inflammation (e.g., gastrointestinal cramping) will present. These waves and their ensuing systemic inflammation symptomatology can persist for as long as 90 minutes. They can be extremely uncomfortable and mentally debilitating depending on the degree of systemic inflammation. But perseverance can prevent hypoxia and tissue damage. Hypercytokinemia may drive a pulmonary hypertension doom loop, exacerbating hypoxemia as explained below in the Appendix.
CLOTTING WAVES: PR quickly ramps from baseline (e.g., 77 BPM) by 40-60% often to tachycardia (e.g., 114 BPM), without any apparent reason, while SpO2 remains stable (e.g., 96%). Inaction generally results in a significant decline in SpO2 within 20-30 seconds. Symptoms consistent with systemic inflammation (e.g., gastrointestinal cramping) usually do not present. These waves typically last for 10-20 minutes. If PR returns to baseline after sitting back down and SpO2 remains elevated, the clotting wave has ended. If PR fails to recover within a reasonably short period of time, clotting remains active and SpO2 will begin to fall again unless aggressive walking is engaged.
Sniffing Cytokines
For as long as I can remember, I have always suffered anosmia (loss of smell) with routine upper respiratory viral infections. What a crazy experience to crack open the Vicks VapoRub, shove my nose in the jar, and smell absolutely nothing! However, even with this complete loss of smell to external odors, I always sensed some weird, chemical-like smell emanating from within my nasal mucosa periodically during the acute phase of the infection. My sense of smell always returned to normal after seven to ten days from initial symptom onset, so I thought nothing more of these near annual experiences. Others have experienced this same phenomenon with severe COVID:
Infected With Delta | My Immune System Tries To Kill Me
The oversized inflammatory response to these common cold viruses presaged how my immune system would react to a Delta SARS-CoV-2 infection this past September. Indeed, despite being in perfect health, having lived a radically healthy lifestyle for decades, immune dysregulation precipitated into severe COVID marked by hypercytokinemia and a stubborn state of hypercoagulability. I chronicled my entire experience, including our household's disease timeline, in this post - Early Treatment With Colchicine, Not Ivermectin, Saved My Life From Severe COVID.
Briefly, in cases such as mine, severe COVID is caused by complement cascade hyperactivation in which complement proteins drive hypercytokinemia which leads to (mostly) pulmonary microvascular thrombosis, marked by rapidly declining oxygen saturation, and possibly fatal macro-thromboembolic events if aggressive anticoagulation therapy isn't pursued.
No Prophylactic Anticoagulation
In the post referenced above, I explain how colchicine mitigated this cytokine syndrome, kept me out of hospital, and eliminated the need for steroids and supplemental oxygen. The downside to this therapeutic success was the fact that I could find no doctor who would prescribe me a very much needed anticoagulant like enoxaparin or rivaroxaban despite having experienced multiple episodes of syncope, likely due to severe hypoxia, after inadvertently falling asleep. The local clinicians were more interested in criticizing me for having used ivermectin earlier in the disease course. And the now famous frontline telemed docs were swamped and remained unreachable. So I was forced to physically anticoagulate myself using my pulse oximeter as my guide.
The Lowly Pulse Oximeter
I began advocating on social media for every household to have at least one pulse oximeter in March 2020 when the world began to understand the symptomatology of severe COVID thanks, in large part, to early reports from frontline clinicians treating Italy’s Lombardy region.
Fortunately, I bought mine months before supply evaporated as the first COVID wave hit the US in early Spring 2020. Conveniently, I had several AAA rechargeable batteries on hand because I wore my pulse ox 24/7 for two weeks straight. Within a day or two of active monitoring, I learned how to differentiate between cytokine release waves and clotting waves.
Seeing A Pattern In Oximetry
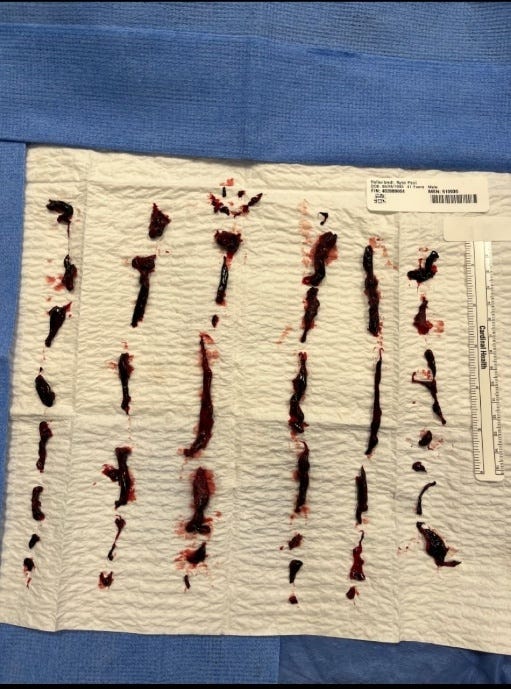
Both physiologic events ultimately manifested in declining oxygen sats (SpO2) and increased pulse rates (PR). And the cure for both was the same - active walking for the duration of the wave. Sleeping through a cytokine wave, although likely resulting in temporary pulmonary hypertension (PH) as explained below in the Appendix, might not be that detrimental to long-term health. On the other hand, sleeping while actively clotting, without having the therapeutic benefit of anticoagulants, could damage lung tissue and lead to permanent impairment or necessitate surgical embolectomy as represented by the picture below received from a friend of a friend - he survived! Certainly the happy face at the top indicates happier lungs post op!
Cytokine Waves
Having spent 1000s of hours researching COVID’s pathophysiology prior to getting infected, I was already well aware of the role proinflammatory cytokines (e.g., TNF-alpha, IL-6, IL-1ß) played in the pathogenesis of severe COVID after the viral replication phase. So when I smelled those same odors from my childhood in my nasal mucosa after anosmia set in, I knew exactly what was happening. Within 20 seconds following the sensation of those odors, the gastrointestinal cramping began, SpO2 declined markedly (e.g., into 80s) from baseline (e.g., 95%) and PR remained stable (e.g., 84 BPM).
If I remained seated, hypoxemia resulted as PR rose within 30-60 seconds in an attempt to restore baseline SpO2, but always failed to do so. These waves and their ensuing systemic inflammation symptomatology persisted for as long as 90 minutes.
The GI inflammation was extremely uncomfortable and mentally debilitating. But I walked continuously through the discomfort and prevented severe hypoxia (SpO2 typically ranged upper 80s to mid 90s) and tissue damage through deep breathing. When the GI cramping resolved, I sat back down and checked the oximeter. Usually, both PR and SpO2 returned to baseline.
These cytokine waves continued throughout the day and night until I achieved stable blood levels of colchicine after seven days of dosing. Until that point, the frequency and severity of these waves corresponded to the pharmacokinetics of colchicine that I dosed twice daily.
Clotting Waves
Typically, clotting during severe COVID only happens in the overnight hours because our clotting factors are most elevated at these times, likely based on circadian rhythm. I faced seven consecutive overnight evenings when my lungs were clotting during the acute phase of my disease course. I resolved to simply remain awake each night by binging Netflix movies after experiencing a couple of frightening bouts of syncope.
I discovered PR quickly ramped from baseline (e.g., 77 BPM) by 40-60% often to tachycardia (e.g., 114 BPM), for no apparent reason, while SpO2 remained stable (e.g., 95%). If I remained seated, SpO2 would begin to decline into the low 90s within 20-30 seconds. Symptoms consistent with systemic inflammation (e.g., gastrointestinal cramping) never presented.
These waves typically lasted for 10-20 minutes. If PR returned to baseline after sitting back down and SpO2 remained elevated, the clotting wave had ended. If PR failed to recover within a reasonably short period of time while seated, clotting remained active and SpO2 would begin to fall again unless I resumed aggressive walking. I stayed up one extra evening just to make sure the risk of clotting had truly ended.
Clinical Proof Of Efficacy
Paroxysmal nocturnal dyspnea experienced post convalescence (a topic for a different post perhaps) led to cardiology and pulmonology referrals. My chest x-ray was completely clear which is atypical in severe cases. Elevated d-dimer and sedimentation rate blood tests prompted a CT angiogram w/contrast to rule out pulmonary embolism. The result was minor ground glass opacities in both lower lobes and some infiltrates in the upper left lobe. O2 sats during this period averaged 95-97% with periods of 99%. A two-week taper of dexamethasone and continued colchicine use (1 mg BID) completely cleared up my lungs and restored SpO2 to pre-infection averages.
Sharing The Experience
After reading about my experiences on LinkedIn, Drs. Mobeen Syed and Darrell DeMello asked me to join their discussion surrounding nonpharmaceutical actions anyone can take during acute COVID. I explain how to properly interpret oximetry data during this clip:
Thankfully, others have replicated my results:
Appendix
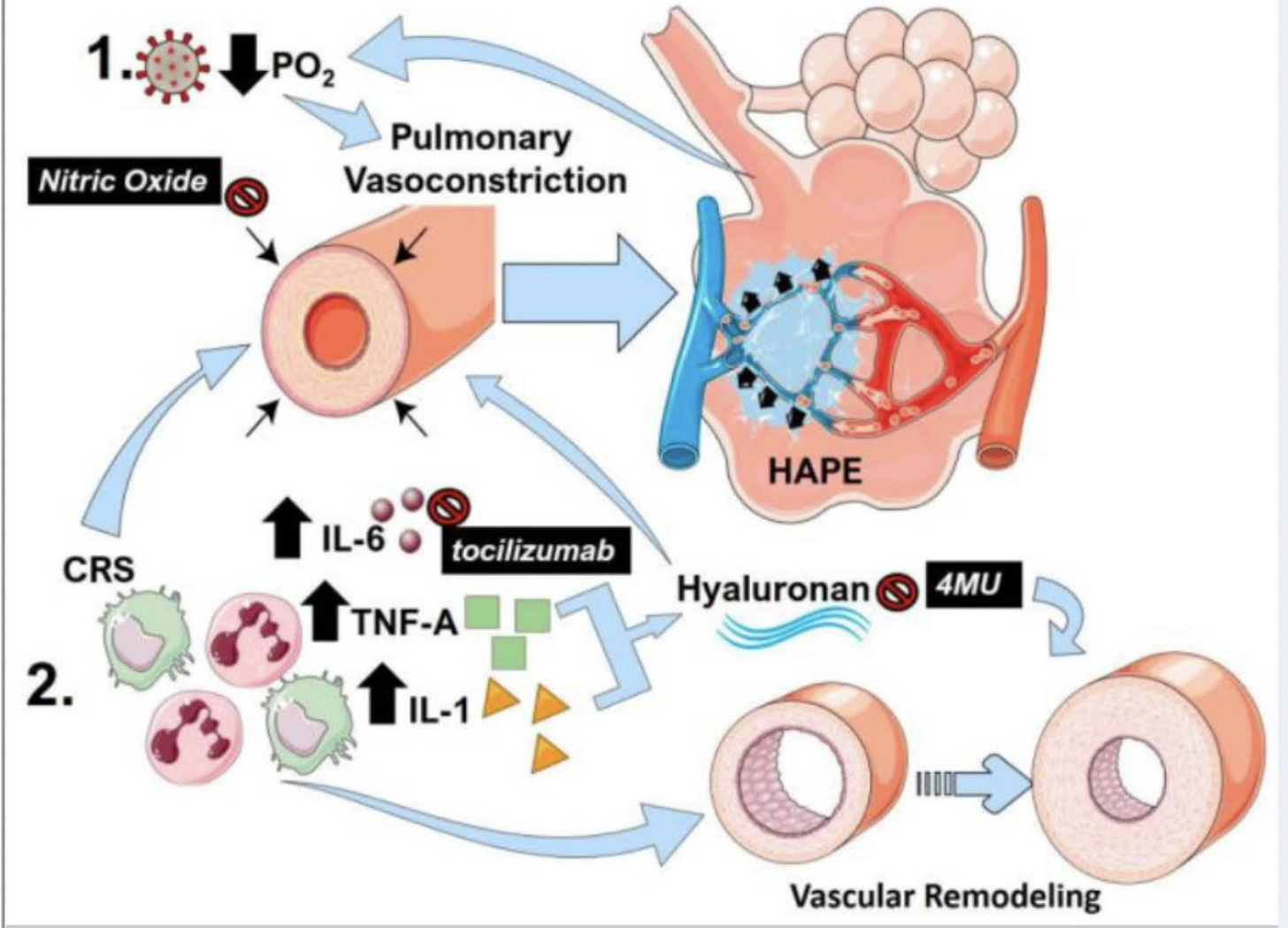
“The link between pulmonary vasoconstriction, high altitude-induced pulmonary edema (HAPE) and the cytokine release storm (CRS) in COVID-19. (1) Following SARS-Cov-2 infection, reduced PO2 and resulting hypoxia can promote sustained pulmonary vasoconstriction, resulting in pulmonary edema akin to HAPE. This in turn results in reduced PO2 that can itself further promote vasoconstriction, resulting in a vicious circle. (2) The cytokine release storm (CRS) in COVID-19 results in an increased in inflammatory cytokines including interleukin (IL)-1 (yellow triangles) IL-6 (brown circles) and tumor-necrosis factor alpha (TNF-A green squares). IL-6 and TNF-A are capable of promoting pulmonary vasoconstriction and vascular remodeling, which are important hallmarks of PH. TNF-A and IL-1 can promote increased hyaluronan levels that also stimulate vascular remodeling and pulmonary vasoconstriction.”





Do you keep your testosterone levels high? The reason I ask is because testosterone drives up levels of a protein called TMPRSS2. (They know this from prostate cancer patients) and they also know TMPRSS2 cleaves the spike protein to initiate membrane fusion. So the more TMPRSS2, the more S1 spike sub-units will be floating around in the blood. And here's a study showing S1 spike subunits causing heart problems.
https://www.biorxiv.org/content/10.1101/2021.06.20.448993v1
The video link on YouTube is no longer available