Early Treatment With Colchicine, Not Ivermectin, Saved My Life From Severe COVID
A timeline of a miraculous therapeutic that kept me out of hospital, off steroids, and off supplemental oxygen.

Summary
Ivermectin prophylaxis did not prevent symptomatic SARS-CoV-2 infection, but it dramatically changed everyone’s disease course for the better
Incredibly aggressive Ivermectin dosing (five days before symptom onset) could not prevent me from experiencing severe COVID
Delta accelerated severe COVID’s pathogenesis by about 50% compared to wild type as I experienced immune dysregulation on day 4 and clotting on day 5, not days 8-10.
Colchicine resolved hypercytokinemia, kept C-Reactive Protein (CRP) in range and reduced d-dimer
I was forced to endure nearly a week of severe COVID symptoms because I unfortunately started the drug after the hyperinflammatory phase had already begun
I was refused anticoagulants (e.g., enoxaparin) while actively clotting overnight and was forced to try to anticoagulate myself through physical activity in lieu of sleeping for six nights straight
I experienced paroxysmal nocturnal dyspnea caused from low oxygen sats and bradycardia after the clotting waves ceased
Dexamethasone and colchicine worked in concert to clear up the lesions and infiltrates in my lungs that presented on CT post convalescence
I ran colchicine for about three months total to completely restore cardiopulmonary functionality
*moved from LinkedIn and updated
It was inevitable. Delta invaded our household the week of September 6, 2021 - one week into the school year for our high school sophomore and senior daughters. Despite wearing stacked N95s inside every foreign indoor airspace since March 2020, my wife and I were nothing less than sitting ducks thanks to the myopia of our local high school district board which decided to abandon all the nonpharmaceutical interventions it had implemented during the previous school year in the face of a contagion that was now several times as infectious as last year's wild type SARS-CoV-2.
Ivermectin Prophylaxis
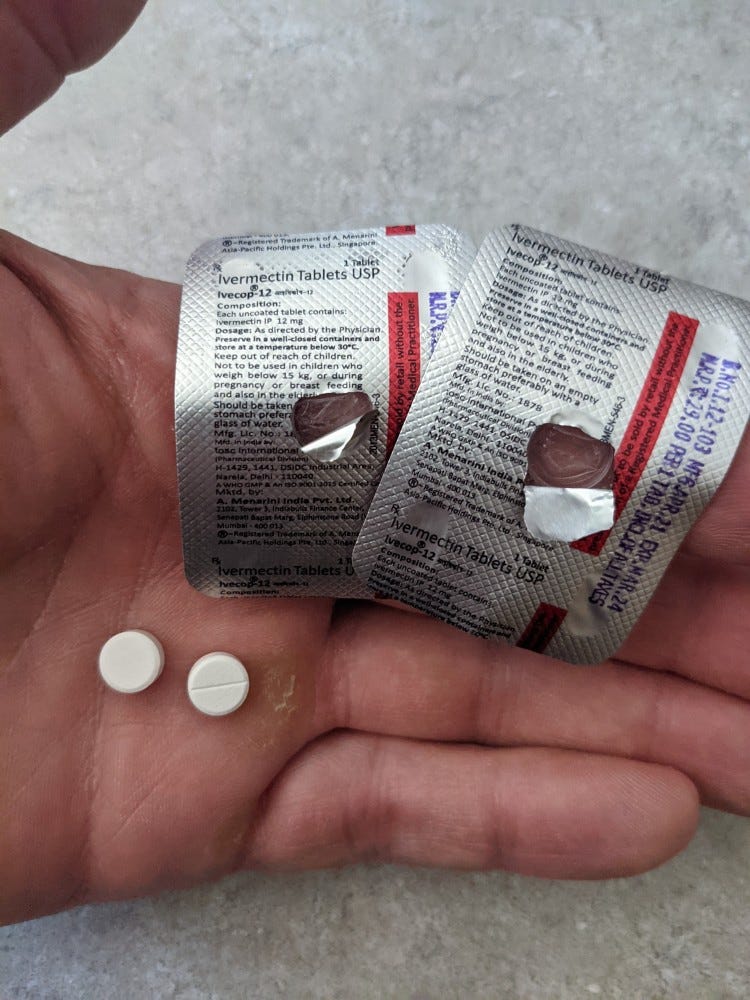
Before the school year began, I emailed the school administration highlighting the fact that the newly adopted COVID mitigation policies (essentially none) for academic year 2021-2022 were completely contrary to CDC's updated guidance for delta. My email was politely dismissed by a reply completely devoid of any established epidemiologic science. Consequently, I began prophylaxing the entire household with ivermectin at 0.3 mg/kg q4d. My rationale was this dosage roughly equaled Dr. Allan Landrito's prophylaxis dosage of 0.5 mg/wk which he claimed on World Ivermectin Day limited breakthrough infections in his Philippines patient base of roughly 100,000.
Ivermectin Prophylaxis Fails 100% Against Delta
Unfortunately, unmasked ivermectin, daily mint Listerine gargles, and Carragelose nasal spray prophylaxis failed to protect our sophomore daughter from getting infected at school. On Friday, September 10, early evening, she complained of feeling "off" during the school week. I immediately took her temperature: 100.4F. At this point, I knew she was infected and the rest of us were likely already infected as well. Her positive PCR that following Saturday morning was merely a formality.
Acute COVID Treatment
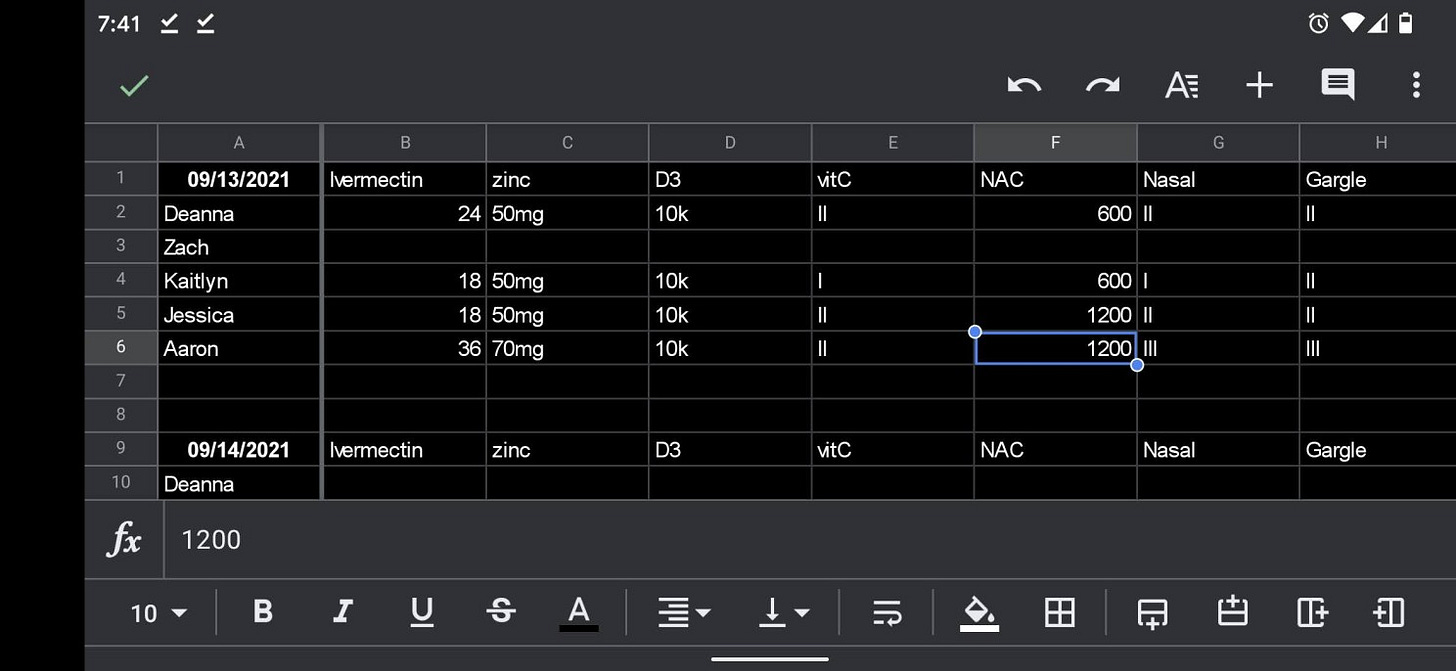
I began dosing all five of us in the household at 0.3-0.4 mg/kg ivermectin daily that Friday evening. Additional therapeutics included 500 mg ascorbic acid q3h, daily sun exposure or 5,000-10,000 IUs cholecalciferol, 600 mg BID NAC, 50-70 mg elemental zinc, and 0.5% povidone iodine gargles and nasal scrubs. I included 250 mg azithromycin BID and 325 mg ASA in the treatment regimen for my wife and me.
Our sophomore daughter tested negative on Sunday, September 19, ten days after her initial fever. Delta was a complete non-event for her.
Delta's 100% Household Attack Rate
Two days after our daughter tested positive (Monday, September 13), my wife presented with allergy like symptoms. Having already decided she would get a monoclonal antibody infusion after FDA lowered the BMI requirement from 30 to 25, we proceeded with getting her tested immediately and contacted her PCP to arrange for the infusion. Two days later, she walked out of a nearby hospital infusion center having received the Regeneron/Roche combo (casirivimab/imdevimab). She experienced one day of fever and had some posterior lower body aches. Eleven days after symptom onset, she tested negative on September 23.
Our high school senior daughter tested negative, and we concluded she had already convalesced from a prior SC2 infection. Our 19 year old son presented with no symptoms. In fact, it wasn't until I placed an oximeter on his finger that I discovered he was in a bit of trouble. Sats were fluctuating in mid 90s but HR was elevated above 100 BPM (tachycardia) at rest. After concluding a week of ivermectin, I began dosing him with colchicine on a two tabs AM/1 tab PM schedule. A 15-day course reversed the inflammation that was affecting cardiopulmonary function. He tested negative on Monday, September 27 and experienced no visible symptoms at any point during his infection.
Premature Declaration Of Victory
After thinking I had avoided delta infection, having run ivermectin for five days straight before any symptoms, I presented with 101.1F fever on the evening of Tuesday September 14. This was disappointing to say the least, especially considering the aggressive daily povidone iodine gargles and nasal scrubs. Apart from the fever, though, I felt great. I experienced no debilitating symptoms. I actually believed I had beat delta in just a few days. However, the sticky fever (as high as 102.3F at times), driven by IL-6, was a presage of the future.
Descending Into Dysregulated Complement Activation
While riding my lawn tractor on Friday afternoon, September 17 (day 4), I noticed I was retaining a significant amount of water in my gut. An hour or so later, something flipped physiologically, and I voided four times in about ninety minutes. What I failed to realize at the time was this was the beginning of the hyperinflammatory phase. The inflamed nerve endings in your intestines cause all sorts of digestive problems, destroy your appetite, and dramatically limit your ability to process both solids and liquids. Avoiding meats and spicy foods while restricting your diet to soft foods predominantly derived from plant based sources is absolutely essential. I concentrated on food very high in potassium to avoid hypokalemia during this period of malnourishment. Ultimately, I shed about 15 pounds in ten days.
Hyperinflammation Drives Coagulopathy
Within 30 hours (Saturday, September 18 - day 5), I was well into the hyperinflammatory stage and actively clotting. The drug that I should have taken several days prior was clopidogrel. Because I didn't have that or enoxaparin, I needed to anticoagulate myself by remaining active during the overnight evening hours - the time when clotting factors are most elevated.
Clotting Waves
I wore an oximeter 24/7 and saw repeated patterns of heart rate and SpO2 that I was able to decode as explained in my Cytokine vs Clotting article. When HR ramped at rest from 70s into 100s-110s while SpO2 remained constant for the first 20-30 seconds, this rapid change indicated active clotting. The only solution I had available to mitigate this risk was to walk fairly aggressively around the house until each clotting wave dissipated. Remaining active prevented the collapse of SpO2 into the 80s even while HR remained elevated. Sometimes these clotting waves persisted for 30 minutes or longer. But they were definitely shorter in duration than the cytokine waves.
I could determine a clotting wave had ended by sitting back down and watching the oximeter. If HR fell while SpO2 remained constant, the clotting wave had ended. If HR remained elevated while SpO2 fell, I had to get back up and resume aggressive walking. This was the procedure I repeated every night from September 19 (day 6) - September 24 (day 11).
NIH Stupidity Pollutes Local Hospital
On Tuesday morning, September 21, at 12:30 am, I walked into a local hospital emergency department and requested a d-dimer test and enoxaparin to preemptively get ahead of the clotting after experiencing multiple episodes of syncope. One evening I woke up on the floor with no knowledge of how I got there.
Thanks to the colchicine, I was sat'ing at 95-97% with HR in the 80s at the hospital. So admission was out of the question in their eyes. The joke of an ED doc on site was more interested in criticizing me for using ivermectin than merely running a $20 blood test that would have confirmed exactly what I said was happening in my lungs.
"There is no role for prophylactic use of anticoagulation therapy in acute COVID," were the words I heard while sitting on the bed. I asked him how many COVID positives NIH had treated. *Crickets* I asked him if he understood the role IL-6, IL-1ß, and TNF-alpha played in the hyperinflammatory and clotting process. *Crickets*
After getting nowhere with the hospital staff, I disconnected myself from the monitors, walked out, and finally accepted the fact that I would have to do this entirely on my own without access to critically important drugs.
Cytokine Waves
Cytokine waves exhibited different oximetry patterns. Unlike the clotting waves, SpO2 would begin to fall while HR remained constant at rest. I was also able to smell the cytokine release in my nasal mucosa even though I had lost a large percentage of my smell (but not taste). I've always been able to smell these cytokines and chemokines in the upper airway ever since I was a child, but I never knew what I was sensing until COVID hit me decades later.
This sensation gave me advanced notice of what was about to happen in less than 30 seconds. This change also prompted me to get up and walk aggressively in order to force SpO2 to recover into the mid 90s to prevent hypoxemia. The gastrointestinal discomfort and tightness during these waves was extremely unpleasant. Unlike the clotting waves, the cytokine waves persisted for as long as 90 minutes each before dissipating. This was the most mentally challenging aspect of dealing with severe COVID because there was no light at the end of the tunnel during the entire week of September 19 - September 24 (days 6-11).
Hydration Is Essential
Remaining hydrated during this period was an all out war. It was impossible to chug 20 ounces of water in a couple minutes because the gut inflammation precluded this option. Instead, I had to sip water continuously for hours on end to prevent dehydration, declining blood volume, and drops in blood pressure. This isn't a problem in a hospital setting because of the banana bags. Continuous IV fluids isn't an option for most of us at home.
One bout of diarrhea on September 24 flanked by a couple days of loose stools (solved by intermittent Loperamide use) forced me to remain awake all night once again to rehydrate myself. I spent six hours drinking deliberately and finally achieved baseline hydration by the morning.
A Ray Of Hope Appears
The cytokine waves occurred day and night and were relentless until Saturday, September 25 (day 12). We celebrated our daughter's 16th birthday with her friends on this day. This was the first day that I was able to fully enjoy as I could actually feel the difference between this day and the prior days and evenings of the past week.
Interestingly, a study on colchicine determined it took eight consecutive days dosing 1 mg daily before stable blood levels were achieved. I was taking 2 mg daily (1 mg BID). So it isn't a stretch to see how I may have achieved stable serum levels by Saturday, September 25 (day 7 of colchicine use).
The fever that had plagued me since Tuesday, September 14 finally broke on Monday, September 27 (day 14). This change represented a significant turning point in my disease progression. I also had routine bloodwork done on this day: CBC w/differential & platelet, thyroid panel, PSA, vitamin D, and comprehensive metabolic. Incredibly, everything came back in range except for CO2 (one point over high limit), albumin (low), and 25(OH)D (over high limit at 128 ng/ml - all from five months' worth of daily sun exposure). Calcitriol was within range at 74.2 pg/ml.
Bradycardia/Tachycardia
Although the cytokine and clotting waves had ended by this point, the heart inflammation, likely causing some degree of sick sinus syndrome manifest by bradycardia/tachycardia episodes, continued to prevent me from getting restful sleep during the week of September 26 - October 2 (days 13 - 19). Specifically, I would catch my HR dropping into the mid 50s while drifting off to sleep. The slight bradycardia caused SpO2 to fall into the upper 80s as I fell completely asleep. In less than two hours, my body would wake me up in a state of delirium likely caused by persistent hypoxia.
These episodes of paroxysmal nocturnal dyspnea were repeated throughout the overnight hours and simply led to even more sleeplessness. Fortunately, the episodes of syncope I experienced the prior week were gone. My average daily sats for this week were 95% with periods of 98-99% during active hours but likely mid to low 80s while sleeping.
Desperate for sleep, I contacted telemed who agreed to refer me to local cardiology and pulmonology consults and a possible sleep study. I met with a cardiologist on Friday, October 1 (day 18) who appeared unconcerned with my symptoms after running an ECG for about a minute. He outfitted me with a Zio monitor - a modern day Holter monitor - to record my heart activities for a week and scheduled a follow-up in three weeks.
The following Monday, October 4 (day 21), I met with pulmonology who ordered more labs (d-dimer, CRP, sedimentation rate) and a chest x-ray. My d-dimer tested at 742 ng/ml (moderately elevated over 500 ng/ml limit), CRP was within range (a testament to colchicine's effectiveness), sedimentation rate was out of baseline high, and CXR was negative. The lab results prompted an order for a CT angio with contrast to rule out pulmonary embolism.
Sleep Remains Problematic
I still experienced paroxysmal nocturnal dyspnea disturbances during this week, but at least I was capturing each event with the Zio monitor, whose data would be cross-referenced with my log entries. Each night, within about 90 minutes of falling asleep, I would wake to a state of delirium likely caused by hypoxia exacerbated by a drop of heart rate into the 40s as the monitor’s data would eventually uncover. I would wake a couple more times during the overnight hours, but not to a state of delirium. At least I was getting some sleep. Average daily sats remained at 95% during daylight hours with periods of 98-99% similar to the prior week.
On Monday, October 4 (day 21), I dropped the colchicine dose from 1 mg BID to 1 mg morning/0.5 mg evening. By Wednesday, October 5 (day 23), my shortness of breath and chest tightness had returned. I immediately returned to 1 mg BID for another five days.
Tachycardia Scare
On Thursday, October 7 (day 24), I experienced my most severe bout of tachycardia. After being fairly elevated all morning (90s - 110s), my HR rose quickly to 161 BPM while I was driving. I nearly dialed 911 on the side of the road after watching a seemingly unending rise on the oximeter. I reached my destination as quickly as possible and laid down on my side to try to encourage HR to fall. It did return into the 70s - 80s within 40 minutes. I returned home and rested until my HR fell back into the 60s after about five hours. Later that day, I received a positive IgM COVID antibody test as expected. Average daily sats for this week increased to 96%, hitting 99% more frequently than the week prior. My appetite returned to full strength this week.
No Pulmonary Embolism
The CT scan with contrast was performed on Friday, October 8 (day 25). No pulmonary embolism was detected. Areas of mild peripheral reticular and groundglass consolidation throughout the right lower lobe and left upper and lower lobes were discovered somewhat expectedly due to the fact that I was denied enoxaparin during the clotting phase.
Better Sleep Arrives
On Sunday, October 10 (day 27). I awoke to find myself sleeping on my back (worst position for oxygen exchange) sat'ing 99% at 55 BPM. This represented a significant cardiopulmonary improvement and illustrated how colchicine continued to clear up my lungs, eradicate the systemic microvascular clotting, and reduce the inflammation of my heart. That morning I was able to walk around the house and maintain a HR in the 70s instead of watching it ramp into the 110s.
Pulmonology Begins Dexamethasone
Consistent with the experiences of tens of millions of Americans, I wasn't able to get proper outpatient treatment during the acute phase. But now that I had “recovered”, all options were on the table across all specialties. The pulmonologist called me on Monday, October 11 (day 28) to discuss his treatment protocol for clearing up my lungs after reviewing the CT from the prior week. He indicated he would prescribe a Prednisone taper.
Knowing that Prednisone and colchicine didn't mix well, I asked him to change the scrip to dexamethasone since I needed to remain on colchicine for the heart inflammation. He agreed to my request and dose adjusted the taper with dex beginning at 6 mg. Even without the dexamethasone, colchicine was continuing to clear my lower airways. The wheezing that had plagued me for weeks had disappeared by Wednesday, October 13 (day 30) even after reducing the colchicine dose by 0.5 mg two days prior. And the chest tightness I had experienced the first time I tried to reduce the colchicine dose was noticeably absent.
I disagreed with both the dosing and duration of dexamethasone given the severity of the lung infiltrates and the concurrent use of colchicine but didn't say anything. Instead, I merely cut the dose in half, beginning with a much more appropriate dose of 3 mg, and modified the duration of the taper from a month to 15 days.
Cardiology On Deck
I mailed the Zio device back to the manufacturer on Friday, October 8 (day 25) so they could extract the week-long data from the device, correlate it with my log entries, and send the final results to the cardiologist.
On Thursday afternoon, October 21 (day 38), I received a notification in my health provider's app that indicated the final report from the manufacturer was available. After reviewing a week's worth of cardiac data, they found two brief runs of supraventricular tachycardia, no atrial fibrillations, and no ventricular arrhythmias or tachycardias (two serious conditions that can instantly kill a person). I cancelled my cardiology appointment for the following day knowing no additional tests or bloodwork would be ordered and no additional therapeutics (e.g., beta blocker) would be prescribed after such positive sinus rhythm results.
Colchicine continued to reduce the cardiac inflammation that drove the elevated morning heart rates. Even though I continued to experience the tachycardia episodes, I noticed a significant reduction in the amount of time required for HR to recover into the 60s and 70s. What had previously taken tens of minutes to hours (worst case) just three weeks prior, took less than 30 seconds under optimal conditions.
Wrapping Up The Dexamethasone
On Monday October 25 (day 42), nearing the end of the dexamethasone taper, I checked HR during my typical mid-morning activities as I always did. Instead of watching it climb into the mid to upper 90s while walking around the kitchen, it remained anchored in the 70s. As my tweet below indicates, the tachycardia was noticeably absent.
So I decided to do a stair climb test and and further test my HR recovery under some aerobic duress. The results were pretty spectacular and can be seen in the video below. Remarkably, HR actually recovered back to baseline instead of elevating even higher at rest. This behavior was completely opposite what I had seen just a couple weeks prior. I decreased the colchicine dose from 1.5 mg daily to 0.5 mg BID the following day.
Follow-Up Blood Work
On Monday November 8 (day 56), d-dimer, CRP, and sedimentation rate were retested. All three returned within range, with CRP utterly collapsing to 0.5 mg/L - likely due to the addition of dexamethasone to the colchicine. Similar to the cardiology follow-up, I canceled my pulmonology appointment after seeing these results knowing there would be no further action warranted in the eyes of the pulmonologist.
Colchicine Taper
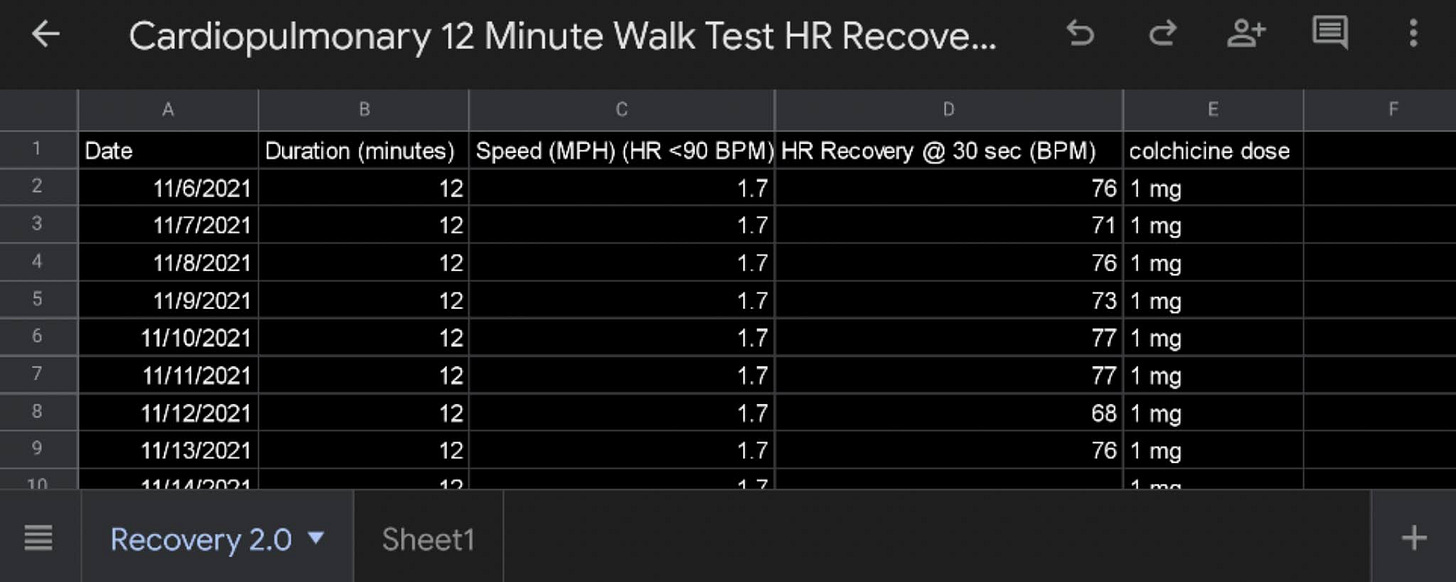
It would take a week or two to fully metabolize the dexamethasone after stopping the drug prior to the follow-up blood tests. So I decided to continue the colchicine at 1 mg daily to complement dexamethasone’s continued therapeutic benefit. I used the controlled nature of a treadmill and the following spreadsheet to track my heart rate recovery trials to assist in colchicine tapering and knowing when I could begin strength training.
Recovery Achieved
On Saturday November 20 (day 68), having witnessed encouraging cardio markers on the treadmill, I decreased colchicine to 0.5 mg daily for the following 20 days and resumed very light resistance training.
What I Learned
First, until you actually endure severe COVID, you cannot truly understand its pathophysiology. Tests help identify what's happening in the body. Radiologic imaging provides additional insight. Therapeutic protocols help standardize care. But the goal should be to limit the initial collateral damage instead of trying to treat the consequences of hyperinflammation and clotting after the fact. In light of this reality, the Western medicine approach of sending COVID positives home with paracetamol to self isolate until they can't breathe is sheer insanity and represents nothing less than medical malpractice in light of proven therapeutic interventions demonstrated globally by clinicians who are actually practicing medicine by treating the patient in front of them instead of heeding the advice of hospital administrators and public health agency representatives who haven't treated a single COVID patient.
Second, severe COVID is not an allergic reaction. It's a pathologic condition driven by dysregulated complement activation in the absence of comorbidities such as metabolic disease. Just because other classes of drugs work doesn't mean they are the best choices. I have a household full of people who suffer from terrible hypersensitivities including mast cell degranulation presenting with cold urticaria and other reactions. Not one experienced even the faintest hint of severe COVID. In fact, there was zero downtime in their daily activities. It was as if they were completely unaffected. I, on the other hand, have never been allergic to anything and have never experienced a hypersensitivity reaction in my life prior to severe COVID.
The following discussion excerpt is taken from the study Increased complement activation is a distinctive feature of severe SARS-CoV-2 infection published in Science | Immunology:
“Here, we demonstrate that (i) markers of complement activation are higher in severe COVID-19 compared with those hospitalized with influenza or other forms of acute respiratory failure; (ii) markers of complement activation distinguish those with worse outcomes in the setting of COVID-19, in two independent cohorts; (iii) the AP (alternative pathway) is activated in patients with COVID-19 and is implicated in these worse outcomes; and (iv) components of the AP associate with markers of endothelial injury and increased coagulation, which are the clinicophysiological hallmarks of severe COVID-19 vasculopathy.”
Further, the severity of the dysregulated complement activation has nothing to do with viral load as concluded by the following study Systemic complement activation is associated with respiratory failure in COVID-19 hospitalized patients
“C4d, sC5b-9, and C5a correlated with antiviral antibodies, but not with viral load.”
Third, ivermectin prophylaxis simply doesn't work at all against delta without adequate and simultaneous PPE use. We had a 100% failure rate in our household while dosing ivermectin at 0.5 mg/kg weekly. Once our daughter presented with symptoms, we all masked (even with N95s indoors), aggressively ventilated the home, and selectively isolated in various parts of the home during the overnight hours. None of this mattered because we had been infected prior to Jessica presenting any visible symptoms.
Fourth, colchicine is the miracle drug against COVID if initiated early enough. Ivermectin definitely helped me clear the virus sooner, but it could not prevent my immune system from precipitating into a very dysregulated state. Colchicine kept me off steroids, off supplemental oxygen, and out of the hospital as my sats generally remained in the mid 90s despite having a very severe case of COVID. In fact, I have friends who received the typical dexamethasone/enoxaparin/tocilizumab stack in the hospital who took months after being discharged to hit numbers I was routinely hitting even during my worst moments of the disease. I didn't need four, six or ten different drugs to fight severe COVID using only colchicine after deteriorating into complement cascade hyperactivation.
The following pharmacologic explanation was written by Alben S. delivered courtesy of Dr. Darrell DeMello:
Why Colchicine works in Covid19 and prevents thrombosis
Thrombosis in vessels occur due to multiple factors, but of them inflammation is the most common. Inflammation activates thrombosis through tissue factor - internal cascade of coagulation. Tissue Factor when exposed to blood interacts with factor 7a to activate factor Xa - the key activator of thrombin. Tumor necrosis factor is a key inflammatory marker and this induces monocytes to produce this tissue factor inside the blood vessels. Once you have activated monocytes producing plenty of tissue factor, you will see intravascular thrombosis. Colchicine is a potent inhibitor of TNF-alpha, thus prevents activation of the monocytes.
Colchicine prevents tubulin formation inside neutrophils, which is needed for neutrophils to migrate to a site of inflammation. In many inflammatory diseases, neutrophils are the pivotal cells involved. Their participation in inflammation depends upon their ability to migrate towards the damaged or stimulated tissues. Since neutrophil migration is affected by microtubules, the interaction between colchicine and tubulin distorts this capability, thereby suppressing the inflammatory process.
Endothelial cells play an important role in neutrophil transmigration towards the inflammatory site; and since colchicine can alter the distribution of adhesion molecules on these cells, it further inhibits the inflammation inside the vessels which triggers the tissue factor and the entire internal cascade of coagulation.
Giving anti coagulants with colchicine not only blocks the Factor Xa activation but also the inducer of Factor Xa and thus colchicine can prevent thrombosis if given as a prophylactic and is protective in infected individuals as the virus induces TNF-alpha which is also subdued by colchicine.
Fifth, credit for my incredible results goes to Dr. Darrell DeMello who guided me through every phase of my disease progression, explained exactly what was happening in my body, and instructed me how to best mitigate against the risk of injury using physical interventions and the therapeutics I had at my disposal. As far as I'm concerned, he has mastered COVID in the outpatient setting. And if the entire world followed his therapeutic strategies, the hospitals would be empty within a few weeks.
Also, credit goes to Dr. Dharmendra Singh who checked in on me daily for several weeks to verify progress. He identified key turning points based on the metrics I fed him. A true wealth of knowledge and clinical experience!














Thank you for sharing the detailed account of your suffering and recovery from the illness.
Hi Aaron,
How can I PM you re: preparing for the inevitably of ME getting COVID in the future? I've lost friends and family for being unprepared who thought a fistful of IVE was all that was needed. I have an Indian pharmacy (I have all the FLCCC meds) but would like another referral for backup in case of confiscation.
Also I have been corresponding with Dr. DeMello and his responses have been $350 for a package of meds delivered at my own risk (which I have no problem with), but after 3 contacts with him and 2 requests asking him HOW I AM SUPPOSED TO COMMUNICATE WITH HIM WHILE SYMPTOMATIC, I have not gotten a response!
How did you manage to actually communicate with him?
I'm also in queue for Dr. Mollie James who Dr. DeMello told me can prescribe in the U.S. and is familiar with his protocol.
Do you have any suggestions?
I am an RN and can generally navigate ok, but months have gone by without finding a successful COVID treatment doctor, and I would desperately like a solution so I can empower myself to assist others to prevent severe sickness and death.